WHAT IS THE NIKAS TEST AND WHICH INFERTILITY COUPLES CAN IT HELP
The “Nikas Examination”, through the analysis of endometrial samples with scanning electron microscopy detects infections, hormonal imbalances, atrophies, hyperplastic changes, and other disorders. Also, with the same examination, the window of implantation (pinopodes) can be assessed.
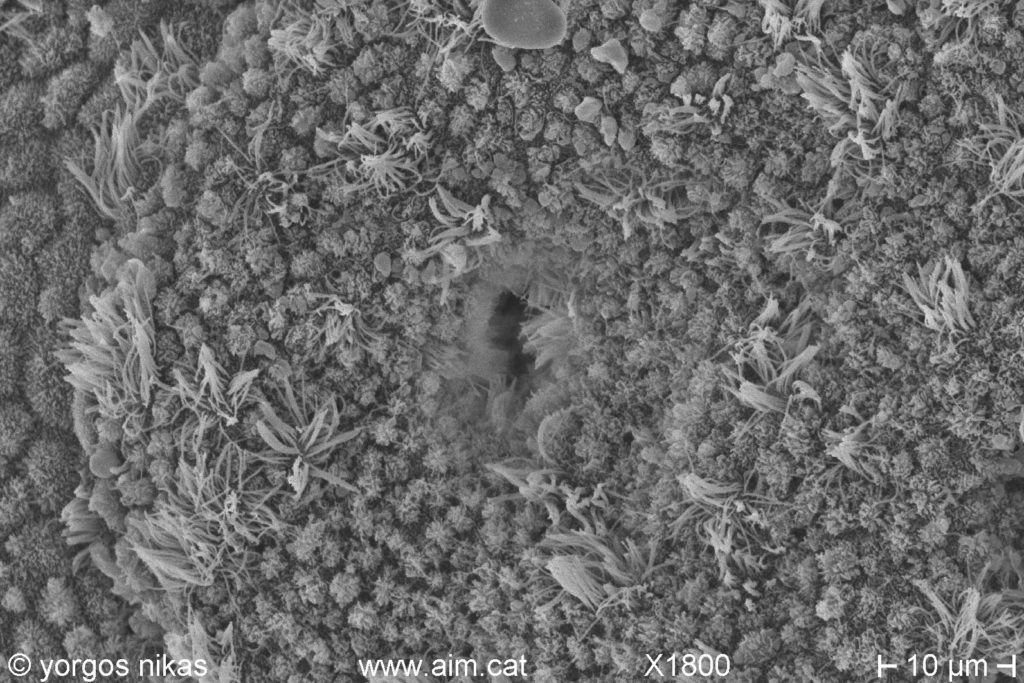
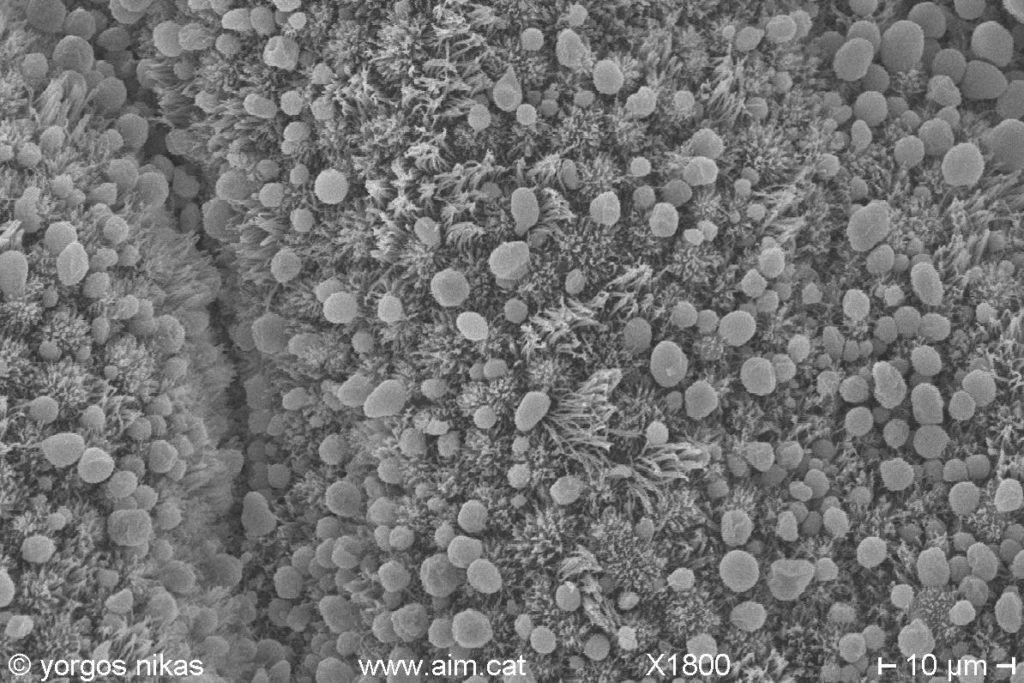
The endometrium, i.e. the inner wall of the uterine cavity, plays an important role in reproduction. One week after ovulation, the fertilized egg that is in the blastocyst stage on day 6 begins to implant in the endometrium, which is now in the receptive phase. Synchronization of embryonic development with endometrial maturation is essential for the initiation of implantation (the so-called window). Penetrating the microcosm of the endometrium with the scanning electron microscope that provides a panoramic view of cell and tissue surfaces, we see that during the receptive phase cell surfaces change dramatically: hair-like microvilli are replaced by larger formations resembling mushroom or flowers, the so-called pinopodes.
From my own studies as well as those of other researchers, it appeared that pinopodes are a reliable marker of endometrial receptivity. Pinopodes appear for only 2-3 days in the mid-secretory phase of the menstrual cycle. The exact cycle days that appear may vary from woman to woman. Examining the pinopodes in women with repeated failed embryo transfers, it appears that in several cases the window “opens” earlier or later than expected.Utilizing this information, the day of embryo transfer was accordingly modified with the aim of optimal embryo-endometrial synchronization, with good results. Following this concept of the personalized window of implantation, other methods of its calculation were later developed, with the molecular “ERA test” being the most prevalent.
This transfer day change has helped many women who had failed in previous attempts to become pregnant. However, there were many more that were not benefited from better embryo-endometrial synchronization. It was clear that something else was to blame for these failures; some factor other than timing was playing a much more decisive role. In recent years, improving the techniques of preparation and visualization of the samples I managed to see under the microscope something that left me astonished!
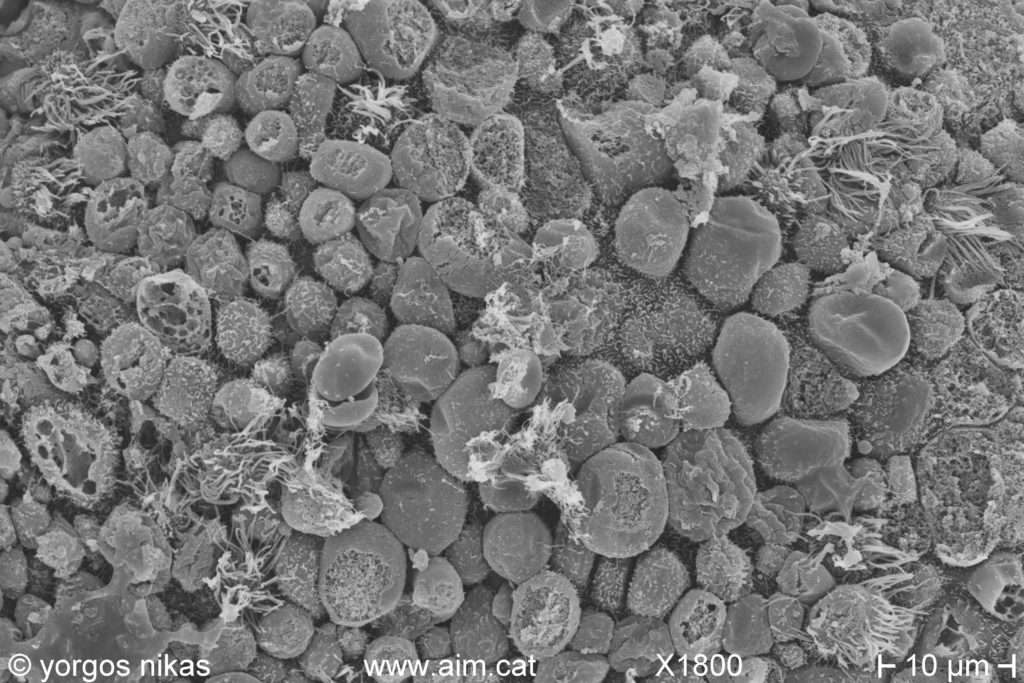
The vast majority of women with a history of repeated implantation failures and repeated miscarriages have inflammation and infection in the endometrium (chronic endometritis) which is often extensive and with intense damages. The cause and mode of onset of chronic endometritis is not clear. Abortions, childbirth, sexual activity and tampon use appear to be related. What is certain is that it is an “ascending” infection, that is, microbes that are in the vagina or cervix, somehow manage to penetrate the uterus and,ascending, can reach the fallopian tubes and block them.
Their chronic stay in the uterus is insidious as it does not give obvious symptoms or signs, but we can suspect it from the following features: dark period color, severe period pain (dysmenorrhea), pain during intercourse (dyspareunia), persistent vaginal infections, frequent urinary infections and of course infertility, either as inability to conceive or as loss of pregnancy in the form of spontaneous abortion.
Chronic endometritis is usually not seen in microbiological or histological tests, so it remains undiagnosed. Histologically, the diagnosis relies on complex immunohistochemical methods with low reliability. Microbiologically, taking a sample is problematic as it is done through organs that have germs,
i.e. the vagina and cervix, with a direct risk of contamination.
Ultrasensitive microbiological methods that detect molecules corresponding to microbes have recently been developed. Apart from the risk of contamination, the detection of these molecules does not imply the natural presence of the corresponding microbes in the endometrium, nor does it provide information on whether they cause damage and to what extent.
Therefore, these results, like the so-called “microbiome” of the uterus, have a rather theoretical value. With scanning electron microscopy chronic endometritis appears “alive” and in all its glory with numerous signs such as the presence of altered mucus and exudate, red and white blood cells, atrophy and degeneration of the tissue, hypertrophic cells and micropolyps and finally with the presence of microbes, often of different species. A quantitative assessment of the extent of the damage is made and any other accompanying alterations are also identified, e.g. those due to hormonal disorders.
The Nikas Test has high reliability, sensitivity and specificity far beyond other when it comes to the diagnosis of endometrial inflammations/infections and of course the evaluation of the therapeutic effect. In addition, with the same examination the window of implantation can be estimated.
Chronic endometritis, like the chronic infections in general, is often persistent and requires prolonged treatment with antibiotics, which may be given for several weeks. An innovation that my colleagues and I managed to develop is the local treatment with intrauterine infusions of intravenous antibiotic preparations and parallel administration of the drugs by mouth.
This combination has no side effects and is much more effective than oral administration alone. The patient may see a sudden improvement in the symptoms and signs of endometritis. The progress of the treatment is evaluated by repeated examination. Since these infections tend to recur, for treatment to be effective it must be immediately followed by an attempt of conception.
Given the enormous frequency (prevalence) of chronic endometritis, I think my test is indicated in all but infertile women as a basic preliminary test along with salpingography. The immediate detection and treatment of any infection in the uterus will help the couple to avoid inappropriate treatments and subsequently, if the conditions are present, to be able to achieve a natural conception. If IVF is still needed, treating any infection will substantially contribute to success.
Unexplained infertility followed by unexplained failure at embryo transfer almost always indicates the presence of endometritis. It is precisely the reason that leads excellent colleagues and embryological laboratories to failure, and countless couples to disappointment and despair around the world.
At the moment my worthy colleagues and I in Greece are leading the world in the diagnosis and treatment of chronic endometritis, a disease that was, is and will be as common in humans as in other mammals, and the enormous impact it has on fertility is yet to be demonstrated in the coming years.
Practical information for the examination
Generally
Endometrial lesions can be assessed on any day between the 8th and 25th of a normal 28-day cycle. Taking before or after should be avoided, as the endometrium shows signs of regeneration at the beginning and degeneration at the end of the cycle. If the biopsy is taken in the mid-secretory phase, the implantation window can also be estimated.
Sampling method
Endometrial tissue collection is easily done in the gynecology clinic with a suction catheter (pipette). Antibiotics can be given prophylactically, starting before the biopsy. The biopsy can be combined with a hysteroscopy, as long as it is taken before the hysteroscope is inserted and always with a pipette.
Maternal cycle and day of reception
-In a simple natural cycle of 28 days, the best day to take a biopsy is the 20th -21st. A progesterone measurement will show if ovulation has occurred.
-If ovulation is monitored, we prefer to take a biopsy 7 days* after ovulation.
-In an ovulation induction cycle we also prefer to take a biopsy 7 days* after ovulation.
-In an artificial cycle with estrogen and progesterone we prefer to take a biopsy on the 7th day** of progesterone administration.
*if e.g. it was Monday, we will take next Monday.
**day 1 is the day we started progesterone.